- Home
- Search
- Browse
- Hot topics
- Matrices
- About
- Help
- Contact
 Matrix cell
Matrix cell

Interventions; Reducing harm
Seminal and key studies on the effectiveness of harm reduction interventions such as needle exchanges.
S Seminal studies
K Key studies
R Reviews
G Guidance
more Search for more studies
Links to other documents. Hover over for notes. Click to highlight passage referred to. Unfold extra text 
S The study which (seemed to have) validated needle exchange in the UK (1989). Published journal article reported “small but encouraging” extra reductions in the HIV risk behaviour of attendees at pilot exchanges in England and Scotland versus a comparison group, legitimating nationwide expansion. But an Effectiveness Bank critique (2004) reminds us of an unpublicised comparison, which was not encouraging at all. For discussion click here and scroll down to highlighted heading in bite’s Issues section.
S Methadone maintenance protects against HIV infection (1993). Over the 18-month follow-up, 22% of US injectors who had not been on methadone became HIV positive but just 3.5% who had remained in methadone maintenance, a “striking” difference attributed partly to their reduced injecting and sharing of injecting equipment. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
S
Methadone treatment saved lives in Sweden (1990). Restrictions on methadone maintenance in Sweden enabled its value to be convincingly demonstrated; when detoxification and drug-free treatment were the alternatives, deaths were about eight times higher. Reviewed with other Swedish studies in The Swedish experience (2000) on p. 6 of linked PDF file.
See later confirmatory studies (1 2) from Sweden, and below similar studies from Norway. For discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
Expand needle exchange and opioid substitute prescribing to contain hepatitis C (2011). Pooled UK data showed that being and staying in methadone maintenance and allied treatments plus adequate access to fresh injecting equipment has prevented many hepatitis C infections. Extrapolating from this data indicated (2012) that to make further substantial progress these interventions must reach not half of UK injectors, but at least 8 in 10. Some of the same authors have collated (2014) studies contradicting previous conclusions that opioid substitute prescribing does not prevent spread of hepatitis C. For discussion click here and scroll down to highlighted heading in bite’s Issues section.
K
US randomised trial confirms that methadone maintenance prevents infection infection risk behaviours (2000). Proving methadone maintenance reduces risk of infection has been hampered by the near absence of randomised trials, hence the importance of this US study contrasting continuing maintenance with detoxification. Despite being compensated for by more intensive psychosocial support, when methadone was withdrawn gaps in infection infection risk behaviour and illicit opioid use opened up favouring the maintenance patients. For discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
Longer on methadone means longer lives for UK heroin patients treated by GPs (2010). GP records suggest opiate users are less likely to die prematurely if substitute prescribing is made available, and that the longer they are in treatment, the greater the life expectancy dividend. This data led to the estimate (2011) that shortening an average nine months of treatment to six would cause 10% more deaths while extending it to 12 would cause 5% fewer. Similar study of specialist services below. For related discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
English study finds staying in specialist substitute prescribing treatment saves lives (2015). Results suggest that to save the lives of people dependent on heroin or similar drugs, they should be engaged and retained in substitute prescribing programmes like methadone maintenance. Shortly after leaving residential/inpatient care was the highest-risk period. Similar study of primary care patients above and below of opiate users in general whether in treatment or not. For related discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
Without treatment there might have been 70% more opioid overdose deaths in England (2015). Estimates that across the entire population of problem opiate users in England, between 2008 and 2011 addiction treatment (mainly substitute prescribing) reduced total opioid-related overdose deaths from what would have been 6372 to 3731. Similar study but confined to treatment patients above. For related discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
Restricted access in Norway exposes substitute prescribing’s lifesaving potential (2008). During their long wait for a slot in Norway’s substitute prescribing programme, five times as many opiate-dependent applicants died due to overdose as did patients in treatment. Similar findings (2013) in respect of drug-related physical complaints. Message is that services should strive to retain ‘problem patients’ in treatment. Similar Swedish studies above. For discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
K
Treatment offers shelter from overdose risk (2008) Reports on a large Italian study (2007) which highlighted the protection against overdose deaths afforded by being in treatment, and the danger of leaving with reduced tolerance to opiate drugs but still vulnerable to relapse.
K
Training drug users to administer overdose-reversing medication (2008). First large UK follow-up study confirmed the feasibility and to a degree the desired impacts of overdose prevention training featuring the opiate-blocking drug naloxone. However, often naloxone was not used (2009) because drug users were reluctant to carry around the pre-loaded syringes, and naloxone training ‘cascaded’ (2011) to other clinicians and patients at a snail’s pace. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
K
Scotland’s pioneering naloxone programme saved lives of released prisoners (2016). In 2011 Scotland became the first country to fund a national policy of distributing the opiate-blocker naloxone to prevent opioid overdose deaths. According to this evaluation it did prevent deaths where this was most likely to be seen – shortly after release from prison. For discussion click here and scroll down to highlighted heading in bite’s Issues section.
K
Welsh pilot study leads to national naloxone programme (2012). The evaluation which led to the Welsh national programme to distribute naloxone to opiate users and their associates to curb rising opiate overdose deaths. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
R Overview of drug-related harms to health and how to reduce them (2005). Reviewed expertly and from a UK perspective, panoramic view of international research on the impacts of needle exchange, prescribing and psychosocial interventions on harms including infections and overdose. Focus is on the conclusions reached by United Nations agencies. For discussion click here and scroll down to highlighted heading in bite’s Where should I start? section.
R
Opiate substitute treatment cuts HIV infection rate (2005). Pooled results from nine studies from across the world offer “strong evidence” that opiate substitution treatment has been associated with a 54% reduction in the risk of HIV infection. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
R
Psychosocial programmes not the way to reduce HIV risk (Cochrane review, 2010). Found no evidence that multiple training/information sessions were any more effective than minimal educational interventions at preventing behaviour which risks HIV infection among injectors or cocaine users. Findings similar (2012) in respect of hepatitis C.
R
Preventing drug-related disease spread in prisons (2009). Free source at time of writing. Having been in prison has repeatedly been associated with increased risk of infection. Review concludes that needle and syringe programmes and opioid substitute prescribing reduce infection infection risk behaviours in prisons without adversely affecting the health of staff or prisoners. Role of substitute prescribing confirmed by another review (2010).
R
WHO finds “compelling evidence” for needle and syringe programmes’ anti-HIV impact (World Health Organization, 2004). But the WHO-commissioned experts also concluded while necessary these programmes are not sufficient; also needed are education, treatment (especially substitute prescribing) and community development. Findings also published in two journal articles (1 2). For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
R
Needle exchange faces the challenge of hepatitis C (2003 and 2004). Four-part series from Drug and Alcohol Findings documents the difficulty needle exchanges have had in controlling spread of hepatitis C and identifies promising practice ingredients. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
R
Needle exchanges will prevent more infections by switching to low dead space syringes/needles (2013). Simulation model suggests that switching injectors from high to low dead space syringes/needles which retain much less fluid can prevent or reverse injection-related HIV epidemics. English study (2017) found low dead space equipment acceptable to injectors but may need to be introduced gradually. Laboratory study (2017) suggests that to prevent spread of hepatitis C, exchanges should focus on needles and syringes rather than other injecting equipment.
R
Feasibility and effects of naloxone distribution programmes (2014). Free source at time of writing. Because lives are at stake no randomised trials were found by this systematic review, but across 19 studies naloxone was administered 1949 times, generally with a 100% survival rate. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
R
Anti-overdose strategies (Scottish Government, 2008). Wide-ranging review including responding appropriately in an emergency, naloxone, ambulance protocols, local collaborations, and information campaigns. Includes fresh data from surveys and interviews in Scotland with drug users and their families and police and emergency services.
R
Safe consumption rooms reduce risk of drug-related harm and promote treatment entry (European Monitoring Centre for Drugs and Drug Addiction [EMCDDA], 2017). European Union’s drug misuse centre reviews three decades of experience and research from Europe and elsewhere on centres where illicit drugs can be used under the supervision of trained staff, facilities increasingly being considered in the UK.
G
NICE endorses needle and syringe programmes (National Institute for Health and Care Excellence [NICE], 2014). UK’s official health advisory body finds needle exchange “an effective way to reduce many of the risks associated with injecting drugs” though there was “insufficient evidence” in relation to hepatitis C. Recommends expansion so every injector has more sterile equipment than they need for every injection. See also related quality standards (NICE, 2012). For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
G
WHO “strongly recommends” needle exchange and maintenance prescribing to combat HIV (World Health Organization, 2014). Consolidates WHO guidance on HIV prevention, diagnosis, treatment and care for key populations including prisoners and people who inject drugs. Strongly advocates universal access of injectors to needle exchange and of dependent opioid users to indefinite, high dose methadone and buprenorphine maintenance.
G
UK government’s advisers call for investment in substitute prescribing to reduce overdose deaths ([UK] Advisory Council on the Misuse of Drugs, 2016). UK’s official drugs policy advisory body concludes that an ageing population of heroin users in poor health has contributed to recent increases in drug-related deaths, and that to hold down the increases government must maintain investment in substitute prescribing. For related discussion click here and scroll down to highlighted heading in bite’s Highlighted study section.
G
WHO says better access to naloxone will save lives (World Health Organization, 2014). WHO judges that “Increased access to naloxone for people likely to witness an overdose could significantly reduce the high numbers of opioid overdose deaths” and makes corresponding recommendations, but also stresses that naloxone provision “does not address the underlying causes of opioid overdose”. For discussion click here and scroll down to highlighted heading in bite’s Where should I start? section, or here for related discussion in Issues section.
G
Increase availability of overdose-reversing drug ([UK] Advisory Council on the Misuse of Drugs, 2012). UK’s official drugs policy advisory body recommends that the opiate-blocker naloxone and related training be made more widely and easily available to drug users and their associates to prevent opioid overdose deaths. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
G
Scottish Drugs Forum naloxone web site. Offers resources, advice, guidance, information and news on programmes featuring the drug naloxone which reverses opiate overdose. Being reconstructed at time of writing. For related discussion click here and scroll down to highlighted heading in bite’s Issues section.
G
Best practice in drug misuse interventions including harm reduction (European Monitoring Centre for Drugs and Drug Addiction [EMCDDA], accessed 2017). Web-based guidance from the EU’s drug policy and practice evidence centre, offering several fact sheets related to harm reduction.
more
This search retrieves all relevant documents.
For sub-topics go to the subject search page or hot topics on harm reduction, overdose prevention, naloxone programmes, and curbing spread of hepatitis C.
 Close Matrix Bite
Close Matrix Bite 
Links to other documents. Hover over for notes. Click to highlight passage referred to. Unfold extra text 
What is this cell about?
Reducing the harms experienced by the user as a result of their drug use, without necessarily reducing use or seeking to overcome dependence. Seemingly a straightforward humanitarian objective, our hot topic on the issue reveals the complications and the intense controversy over an approach that seems to imply – and in practice requires – a degree of acceptance of illegal drug use. Fundamental questions include what and whose harms we accept as legitimate intervention targets.

Street poster from England in 1989.
Among the harms in practice focused on are infectious diseases spread by shared injecting equipment, in particular HIV – the disease which generated modern-day harm reduction in Britain  illustration – but also hepatitis B and C, and the prevention of ‘overdose’ fatalities.
illustration – but also hepatitis B and C, and the prevention of ‘overdose’ fatalities.
Typically, harm is reduced by changing how drugs are used. Common interventions include needle exchanges which try to ensure that only infection-free injecting equipment is used, and education and skills training to help users avoid particularly risky practices. Substituting a legally prescribed drug of the same type for the original (and usually illegally obtained) substance often has both harm reduction and treatment objectives and effects; research on these approaches is also to be found in cell A3. Harm reduction activities may take place in a criminal justice context and services may prioritise preventing harms to the community rather than to the drug user, issues addressed also in cell A5.
The current cell is well stocked compared to succeeding cells in the row, reflecting the greater research emphasis given to testing interventions as opposed to the impact of the practitioner delivering them (cell B1), how they and the service are managed (cell C1), the strengths and ethos of the service-providing organisation (cell D1), and the entire service network (cell E1). This should not be taken to mean interventions are primary and the other influences secondary. Systems of interacting services and initiatives synergistically reduce harm to an extent beyond the reach of any one type of intervention. An example is how methadone maintenance reduces the number of injections, making it easier for needle exchanges to meet the remaining need for injecting equipment, while exchanges act as conduit into treatment. Simply providing a harm reduction service is no guarantee it will reduce harm; how services are run is critical. Examples include high doses in substitute prescribing rather than a mentality of trying to get to a drug-free state, and liberal dispensing of injecting equipment rather than the more disciplinarian approach of insisting on the corresponding return of used equipment.
Where should I start?
First survey the territory from the vantage point offered by a panoramic review from a UK perspective, one of a series funded to provide “rigorous, independent” assessments of the effectiveness of drug policies. Its trio of authors have long experience researching, reviewing and working in the UK drug sector, including at national policy level, and reinforce the credibility of their conclusions by referral to the findings and recommendations of agencies of the United Nations. They lay out the intervention options (needle exchange, drug consumption rooms, methadone and heroin prescribing, media campaigns, outreach and psychosocial interventions) to reduce harms specifically to health (viral and bacterial infections and overdose), consider each of the harms and interventions in turn, specifically address harm reduction in prisons, and consider the main challenges to implementation, prominent among which is “ideological unease at being ‘soft’ on drug users”.
The World Health Organization’s strong recommendation in 2014 that “People likely to witness an opioid overdose should have access to naloxone and be instructed in its administration” is the main development the review would have been sure to include; otherwise evidence has accumulated but the policy and practice implications have not changed much since its publication in 2005.
Highlighted study
Ironically, one of the European nations most resistant to prescribing heroin-type drugs to dependent heroin users has for that reason been able to most convincingly demonstrate its value. Restrictions on methadone maintenance in Sweden made it possible to allow or deny this treatment effectively at random.
Swedish restrictions levelled the playing field between methadone and other approaches
In states such as the UK, where patients can readily choose to start treatment, their progress compared to drug users not on methadone might be due to pre-existing differences rather than the treatment itself. Swedish restrictions levelled the playing field between methadone and other approaches to a degree not possible where methadone was readily available.
The single most important study tracked patients admitted to Sweden’s national methadone programme before a five-year ban on enrolling new patients. Their fate was compared to that of addicts eligible for the programme, but who did not get in before the ban or had randomly been denied entry. All this comparison group availed themselves of Sweden’s well developed detoxification and drug-free treatment services, yet over on average the next six years, 4 in 10 had died. Over about the same period, only around 1 in 8 of the methadone patients had died. Overwhelmingly, opiate overdose was the main reason for the difference.

This seminal and still highly significant study was followed by others with the same implications. Published in 2009, another Swedish study found that the annual death rate was 1% while patients were on methadone but 2% among untreated opiate misusers. During an enforced break in treatment, hospital admissions rose only to fall again when the same patients were allowed to return, strong evidence that treatment was an active ingredient in avoiding illness and death. In 2010 a further study showed what Sweden could have done had it expanded its maintenance programmes more widely and sooner. It found that a major expansion in provision and easing of restrictions between 2000 and 2006 were associated with and may have contributed to declines in opiate-related deaths and hospitalisations  chart.
chart.
The same message has come from neighbouring Norway, which also has restricted access to methadone. There a study traded on the typically five or six months patients had to wait before they could get a slot at a clinic. All the study’s participants had applied for and been assessed as qualifying for this treatment, yet many were forced to wait, enabling researchers to assess the impact of being denied immediate treatment, itself a guide to what might have happened to all the opiate users had there been no treatment to wait for.
Compared to immediate treatment, the results implied that for each 100 people made to wait for maintenance, an extra one or two will die per year. In line with other studies, the bounce back to pre-treatment overdose death rates after leaving treatment supports a view of methadone and other substitute prescribing programmes as an on-off switch. People in need of this treatment generally quickly improve when it is ‘switched on’, but rapidly relapse once it is off, and especially if it is switched off against the patient’s wishes. Despite this, over the span of the study in-treatment gains overshadowed post-treatment reverses, leaving a substantial net benefit.
Also in Norway, the rebound effect emerged in another study. Even when some illegal drug use continued, being in methadone or buprenorphine treatment dramatically cut hospital admissions due to drug-related physical complaints, but these rebounded when patients left, often forced out due to ongoing drugtaking, opposition to programme rules and controls, or instability in taking their medication.
Given the lack of randomised trials – now impossible due to proof that denying substitute prescribing will lead to avoidable deaths – the Scandinavian evidence is the best we have. But there is at least one randomised trial with similar implications. From the USA, it showed that continued maintenance curbs risk of infection and sustains reductions in illicit opioid use more effectively than gradual detoxification, even if during and after that patients are well supported.
Issues to consider and discuss
 What would have happened if we’d been told the whole story about pilot needle exchanges in Britain?
To test this then controversial anti-HIV strategy, in 1987 the UK government commissioned an investigation of 15 pilot needle exchanges. Two years later a report in the journal AIDS announced “small but encouraging” reductions in the HIV risk behaviour of exchange attendees versus other injectors who had not attended exchanges – enough to legitimate nationwide expansion. However, the study as a whole, and especially its public presentation in the journal, were seriously flawed. Had the whole truth been revealed, the UK might not have developed the widespread needle exchange provision commonly credited with avoiding HIV epidemics seen elsewhere.
What would have happened if we’d been told the whole story about pilot needle exchanges in Britain?
To test this then controversial anti-HIV strategy, in 1987 the UK government commissioned an investigation of 15 pilot needle exchanges. Two years later a report in the journal AIDS announced “small but encouraging” reductions in the HIV risk behaviour of exchange attendees versus other injectors who had not attended exchanges – enough to legitimate nationwide expansion. However, the study as a whole, and especially its public presentation in the journal, were seriously flawed. Had the whole truth been revealed, the UK might not have developed the widespread needle exchange provision commonly credited with avoiding HIV epidemics seen elsewhere.
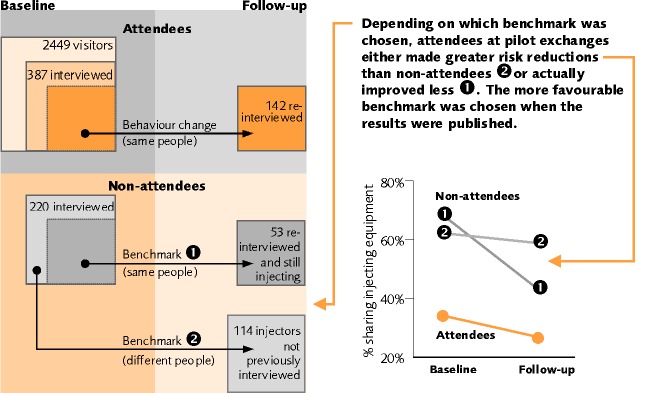
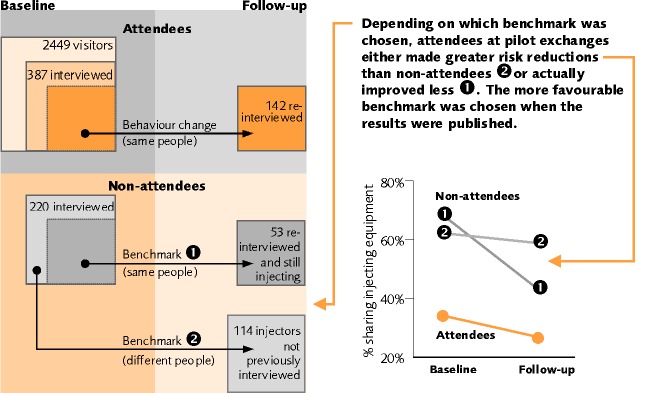
What was the problem? Turn to our analysis for the detailed story. In brief, the pilot exchanges neither attracted high-risk injectors nor could it be shown they reduced risk. Unexpectedly, few injectors who tried the exchanges repeatedly returned, meaning very few were recruited to the study and followed up. The impression that they had reduced their risk more than non-attendees was based on a tiny proportion of exchange users, and on a benchmarking comparison group (numbered 2 in the figure above) which in fact was not comparable at all.
Omitted from the journal article was another, more appropriate comparison group (numbered 1 in the figure) of non-attendees. Like the attendees, they were the same people re-interviewed three months later, not a different set of injectors freshly recruited.
Had the whole truth been revealed, the UK might not have developed widespread needle exchange provision
Without ever attending a needle exchange, they had actually reduced their risk behaviour more than the exchange users – a result which jeopardised the continuance of needle exchange provision.
Both comparisons were there in typewritten black and white in the technical research report, but the published journal article referred only to the more encouraging comparison, and seemed to flatly deny the existence of the one which suggested exchanges were counterproductive. A mistake, a misunderstanding, or an example of the well known ‘researcher allegiance effect’ – the tendency for researchers committed to an intervention to report good results?
In retrospect, it is no surprise that the pilots failed to attract and retain or influence their generally fleeting attendees. Our series on hepatitis C and needle exchange cited the observation that exchanges often choose to or are forced to operate under “restrictions that condemn the programmes to fall far short of the needs of the persons for whom they were designed”. By under-resourcing and undervaluing this work and forcing exchanges to operate under crippling restrictions, sceptical authorities create the conditions which justify their misgivings. Click to  unfold the supplementary text, and you will see there was more than a hint of that in the restrictions placed on the pilot exchanges.
unfold the supplementary text, and you will see there was more than a hint of that in the restrictions placed on the pilot exchanges.
Supplementary text. Click to close 
Implemented to the letter the requirements on the pilot exchanges would make it impossible for the injectors to gain quick and easy, in-and-out access to the equipment they came for. They were required to return used equipment before they would be issued new supplies and the aim was to be one-for-one exchange. Equipment was to be issued only if after assessment and counselling, the attendee remained “unwilling or unable” to stop injecting. The pilot schemes had to keep records of clients, treatment given, syringes issued/returned, and to complete questionnaires with each client on their attitudes and behaviour with regard to drug use, injecting practices, and sexual activity. Some government ministers and the coordinator of the Welsh AIDS Campaign had feared the issued syringes would simply be shared and do nothing to prevent the spread of AIDS, so questionnaire replies on injecting practices were needed as reassurance. Despite arrangements to prevent this happening, injectors were not unreasonably concerned that police would see the centres as handy places to pick up drug offenders.
Problems in Scotland were acute, fanned by professional and political resistance to needle exchange. Dundee’s first scheme effectively ceased operation within months due, reportedly due to under-resourcing causing unacceptable stress among the staff. There were also complaints from other clinic patients about the behaviour of the scheme’s users. Another Dundee scheme opened and tried to absorb the first scheme’s customers, but it too soon closed after threatening and poor behaviour by attendees. Underlying these problems there and elsewhere was the attempt to run needle exchange alongside an abstinence-orientated therapeutic programme, creating tensions for staff and clients alike.
All the Scottish schemes were also hampered by restricted opening hours (in Glasgow, just two afternoons a week) coupled with guidelines originating from the Scottish Home and Health Department limiting the schemes to supplying no more than three needles a time on an exchange basis. Together these restrictions made it impossible for heroin addicts to use fresh equipment each time.
 Close supplementary text
Close supplementary text
If not intentionally set up to fail, the 15 pilot schemes faced restrictions and conditions which would probably, and in some cases, inevitably, lead to this result – one reflected in the bottom-line finding of the evaluation obscured from public view. Whatever the reason for that omission, the effect was arguably beneficial. Many people are alive and disease-free today who would not have been had the exchange strategy been abandoned. We now know enough to be confident that despite the evaluation’s findings, exchanges run on the right lines can help curb disease spread. Where do you stand on this issue? Should the evaluation results have been fully reported, even if that might have meant the end of needle exchange in Britain? As elsewhere, it would have been a case of those not committed to the core principles of harm reduction creating a self-fulfilling prophecy by shackling and under-resourcing the facilities.
 Has methadone maintenance intercepted the spread of hepatitis C?
For decades (see for example a seminal US study) we have known that methadone maintenance can reduce transmission of the HIV virus. In respect of hepatitis C, the consensus has been quite different, but seems recently to have changed.
Has methadone maintenance intercepted the spread of hepatitis C?
For decades (see for example a seminal US study) we have known that methadone maintenance can reduce transmission of the HIV virus. In respect of hepatitis C, the consensus has been quite different, but seems recently to have changed.
In 2003 we explained that what made this virus so much harder to contain than HIV was “the degree of behaviour change needed to intercept its transmission. Reductions in risky sharing of injecting equipment can be enough to minimise the spread of HIV. For hepatitis C, the emphasis is less on reduction, more on elimination … The challenge posed by the virus arises from a combination of robustness, infectivity and prevalence.”
“Prevalence” refers to the critical fact that “the virus took hold before anyone knew it existed and well before anti-infection measures were implemented in response to HIV”. Before in 1989 a diagnostic test was available, it had already infected a much larger fraction of drug injectors than HIV ever would, making it more difficult to achieve the same proportionate reduction than if the starting point had been lower. Since then it has been a case of playing catch-up against a rapidly moving target.
Against this background, over 2003 and 2004 our series on hepatitis C focused on needle exchange because methadone maintenance – the only other drug service to attract large numbers of injectors – “has a convincing record on HIV but has yet to be shown to significantly curb hepatitis C. Usually it is entered too late to prevent most patients already being infected and has at best only a moderate impact on risk behaviour.”
Recent studies – not least in the UK – have forced that generally accepted dismissal of substitute prescribing to be reconsidered. By 2011 the evidence had tilted towards substitute prescribing, but remained too insubstantial and inconsistent to be relied on. Nevertheless, findings from the eight studies gathered together then in a review cumulated to the near-significant estimate that the chances of injectors who received opioid substitution treatment becoming infected were 40% less than those of comparison injectors. That this might not have been an artefact of more harm-reduction oriented injectors choosing to enter treatment was indicated by the fact that other types of treatment were not associated a similar reduction. An important harbinger of later findings was that staying in substitute prescribing seemed more effective than having been in and left, or going in and out of the treatment.
By 2014 later studies not included in the review were seen by a quartet of influential researchers from Britain, Australia and the USA as having decisively tipped the balance in favour of substitute prescribing. Their unqualified conclusion was that opioid substitution treatment “averts infections” with hepatitis C. They also felt it “may also have an accumulating effect – the longer the average duration … the greater the impact on reducing [hepatitis C] risk and drug related mortality”.
By 2014 studies had decisively tipped the balance in favour of substitute prescribing
Listed above and among the studies they cited was a synthesis of results from UK studies. Published in 2011, it estimated that when injectors were engaged in substitute prescribing for at least half of a 12-month follow-up period, the chances of their becoming infected with hepatitis C were less than half those of other injectors – substantial, but still not a statistically significant difference. The following year this data was fed into a simulation model which suggested that current high coverage levels of opioid substitute prescribing may have contributed to reducing chronic hepatitis C prevalence from 57% to 40%. Risk of transmission was lowest if opioid injectors engaged in both high-coverage needle exchange and substitute prescribing, but engaging in just substitute prescribing was estimated to reduce this risk by half – again substantial, but still this estimate could not confidently be declared to represent anything other than a chance finding. Unfold  the supplementary text for more on the studies which by 2014 had led to the conclusion that opioid substitute treatment can help prevent the spread of hepatitis C.
the supplementary text for more on the studies which by 2014 had led to the conclusion that opioid substitute treatment can help prevent the spread of hepatitis C.
Supplementary text. Click to close 
Other UK studies include one from Scotland based on needle exchange attendees. Compared to patients who had left methadone treatment in the last six months, those still on methadone had about 70% lower odds of having recently become infected, though these results also fell short of statistical significance.
Outside the UK, an analysis
of three Canadian surveys of user of illicit drugs found that the prevalence of hepatitis C was significantly lower among those already on or who entered methadone maintenance (24%) than among other participants (76%). More to the point, once other risk factors had been taken into account, methadone patients were also half as likely to become infected over the next two years, and less likely still the longer they had been in treatment during that time. In this study very few survey respondents were in methadone treatment. The analysis adjusted for other influences on risk of infection including whether and which drugs respondents injected, but still this minority may have differed from the non-treatment majority in ways which would have reduced their risk of infection, regardless of treatment.
In San Francisco young adult injectors were almost a third less likely to have become infected if they had recently been in substitute prescribing treatment, a statistically significant difference not found in respect of other treatments and which remained after adjustments were made for other risk factors. Part of the reason for this link seemed to be that opioid maintenance treatment reduces the frequency of injections, and with this the opportunities for viruses to be transmitted.
Australia offered further evidence in the form of a study of injectors who mainly injected opioids. It compared the incidence of new infections among those who at follow-up interviews said they had versus had not be in opioid substitute treatment. After adjusting for other risk factors, those who had not were nearly six times more likely to have become infected, a statistically significant result.
All these were, however, not randomised trials but observations of normal (non-)treatment processes. An unusual example of how non-random allocation can produce misleading findings comes from the one study in the review cited above to find methadone maintenance associated with more injectors becoming infected with hepatitis C. It was set in a general practice in Melbourne, Australia, which did not routinely re-test its continuing methadone patients for the virus. Probably, say the researchers, many patients were not re-tested because the clinic saw no reason to do so. Those who were re-tested would tend to be the higher risk cases – hence the impression that methadone treatment generated infections.
 Close supplementary text
Close supplementary text
Some of the apparent infection reductions found in these studies were very large, but with ethical and practical considerations prohibiting the randomised denial of substitute prescribing, the results might have been due to influences other than treatment. Studies do their best to compensate for known influences, but cannot compensate for those not measured. Set against this is the common finding that treatments other than substitute prescribing are not (or not to the same degree) associated with a reduced chance of becoming infected with hepatitis C; if entering treatment was a marker of a pre-existing tendency to avoid infection, it should apply to all treatments, yet only substitute prescribing has developed a consistent record. Despite the difficulties, the evidence was enough to convince European Union and UN authorities that substitute prescribing should be a major component of anti-infection policies.
How convinced are you? Have we late in the day come to realise that the typically imperfect drug use reductions generated by maintenance prescribing are enough to slow the spread even of hepatitis C? Or is the evidence still too circumstantial? If maintenance prescribing was required to meet the same criteria as a new cancer treatment, would ‘associations’ be enough without the reassurance of randomised trials to establish causality? Or do we have accept that such trials have become impossible, so we must act on the basis of less conclusive evidence or risk avoidable infections and deaths among drug injectors? Note that we do have at least one randomised trial which showed that continued methadone maintenance reduces behaviour risking infection more effectively than gradual detoxification, even if during and after that patients are well supported.
 How much of a difference has naloxone made?
Naloxone is a drug which specifically targets overdoses involving opiate-type drugs – still by far the major contributors to the deaths – rapidly reversing their effects, including the respiratory depression which causes overdose. Worrying increases in overdose deaths between 2013 and 2015 in every nation in the United Kingdom – which got even worse the following year (1 2) – focused attention on programmes to distribute the drug and train drug users and others to how to use it, but also raise fears that these programmes are not yet having the intended impacts. If there is a litmus test in the UK, it is the performance of the determined national naloxone campaign in Scotland, examined below.
How much of a difference has naloxone made?
Naloxone is a drug which specifically targets overdoses involving opiate-type drugs – still by far the major contributors to the deaths – rapidly reversing their effects, including the respiratory depression which causes overdose. Worrying increases in overdose deaths between 2013 and 2015 in every nation in the United Kingdom – which got even worse the following year (1 2) – focused attention on programmes to distribute the drug and train drug users and others to how to use it, but also raise fears that these programmes are not yet having the intended impacts. If there is a litmus test in the UK, it is the performance of the determined national naloxone campaign in Scotland, examined below.
Detailed in our hot topic on the issue, providing naloxone became the main new hope for curbing the death rate after in 2005 UK law was amended to permit emergency
Providing naloxone became the main new hope for curbing overdose deaths
administration by any member of the public, and further relaxed in 2015 to permit drug services in England and Wales without prescription to order supplies and distribute these to drug users at risk of overdose or to people likely to be in contact with them, such as families, carers or hostel staff.
As an intervention, widespread training of potential onlookers to administer naloxone in case of overdose seems close to a sure-fire solution to this leading cause of sudden death among drug users, but as often the case, implementation rather than efficacy is the weak link. The most determined implementation drive in the UK has been in Scotland. Launched in 2011, in 2015/16 7214 kits had been issued in the community and 932 to prisoners about to be released. Whether this programme had the intended effects will influence developments across the UK.
An extremely high-risk period for former opiate users, in Scotland the proportion of opioid-related deaths occurring within four weeks of release from prison had been identified as the key indicator of success of a programme which had specifically and systematically targeted prisons. This was made the main metric in a study listed above which compared opioid-related death rates in the five years before the programme’s implementation (2006–10) with those during its first three years (2011–13). A secondary indicator of success added in the proportion which occurred during the corresponding period after discharge from hospital, another high-risk period.

As the number of naloxone kits issued in prison increased, post-prison deaths accounted for a diminishing % of all opioid-related deaths in Scotland.
The post-prison period accounted for 9.8% of opioid-related deaths before the programme but 6.3% after – a 36% reduction taken as indicative of a lifesaving impact  chart. Also reduced was the combined total of post-prison and post-hospital deaths as a proportion of the total. Routinely collected statistics indicated that the trend down in the proportion of opioid-related deaths occurring shortly after release from prison continued into 2014, when the figure was 3.1%, having steadily decreased since the start of the national naloxone programme.
chart. Also reduced was the combined total of post-prison and post-hospital deaths as a proportion of the total. Routinely collected statistics indicated that the trend down in the proportion of opioid-related deaths occurring shortly after release from prison continued into 2014, when the figure was 3.1%, having steadily decreased since the start of the national naloxone programme.
However, trends in deaths after release from hospital gave no corresponding indication that the programme had helped. Together with the increase in total opioid-related deaths between 2014 and 2016, it calls into question whether overall the programme has had the desired effects, even if it further reduced the small minority of deaths which occur after release from prison.
Reliance on post-prison opioid-related deaths to demonstrate the programme’s success in turn relies on evidence that the systematic targeting of prisons to issue kits actually worked, and produced more complete and/or higher quality implementation than outside prisons, accounting for the reduced proportion of deaths occurring on release. Read our analysis and see if you agree that this proposition is questionable, and with it the decision to use the proportion of opioid-related deaths occurring after prison as the main yardstick of the programme’s success.
It is implausible that such widespread distribution of naloxone and training for its administration did not save lives. The difficulty is in proving this against a background of what is presumed to be upward pressure on the deaths total due to the ageing of the heroin-using population.
 Close Matrix Bite
Close Matrix Bite 







 Open Matrix Bite guide to this cell
Open Matrix Bite guide to this cell 
 Close Matrix Bite
Close Matrix Bite